MENOPAUSE
Menopause, which signals the end of fertility, can be a trying time in a woman's life. When the ovaries stop producing estrogen and progesterone it brings on some difficult physical and emotional changes. Menopause is a topic some women would rather ignore than explore. Many younger women see it as "Irrelevant", but when they approach the age of menopause, they look around for reassurance, that it is not only survivable, but something to look forward too.
What is Menopause?
Menopause literally means permanent cessation of menses. The medical definition of menopause is the absence of a woman's menstrual cycle for a period of 12 consecutive months or longer. Menopause occurs when the function of the ovaries stops permanently, resulting in a loss of hormones estrogens and progesterones, which used to act on the uterine wall leading to a permanent stoppage of menstruation. Menopause marks the end of child bearing potential in a woman.
What is the age when menopause should occur?
The average age of natural menopause in western world is 51, while for Indian women is 48. This is only the average age, with a wide range of 40 to 55 years. Few women experience premature menopause (before 40 yrs) while some experience delayed menopause (>55 yrs).
What is Peri-Menopause?
Perimenopause, or menopause transition, is the stage of a woman's
reproductive life that begins 8 to 10 years before menopause, when the ovaries
gradually begin to produce less estrogen. It usually starts in a woman's 40s,
but sometimes, can start in the 30s as well. During this period, the menstrual
cycles are usually irregular and delayed.
Perimenopause lasts up until menopause, the point when the ovaries stop
releasing eggs. In the last one to two years of perimenopause, the reduction of
estrogen accelerates. At this stage, many women experience menopausal symptoms.
Can I get pregnant if I am perimenopausal?
Yes. Despite a decline in fertility during the perimenopause stage,
you can still become pregnant. If you do not want to become pregnant, you should
continue to use some form of birth control until you reach menopause (you have
gone 12 months without having your period).
For some women, getting pregnant can be difficult once she is in her late 30s to
early 40s due to a decline in fertility. But, if becoming pregnant is the goal,
there are fertility-enhancing treatments and techniques that can help you get
pregnant.
What are the ways in which menopause can take place?
-
Natural menopause Occurs naturally with age
-
Induced menopause Occurs when ovaries are surgically removed at the time of hysterectomy or when the ovaries are damaged with chemotherapy or radiotherapy.
What are the other factors influencing the timing of menopause?
-
Genetic - Some women experience menopause at the same age as their mother or sister.
-
Body structure. Obese women have late menopause than thin women, due to higher circulating estrogens.
-
Gynecological Disease- Women with gynecological disease like fibroids, endometriosis have delayed menopause
-
Cigarette smoking - women who smoke tends to have slightly earlier menopause.
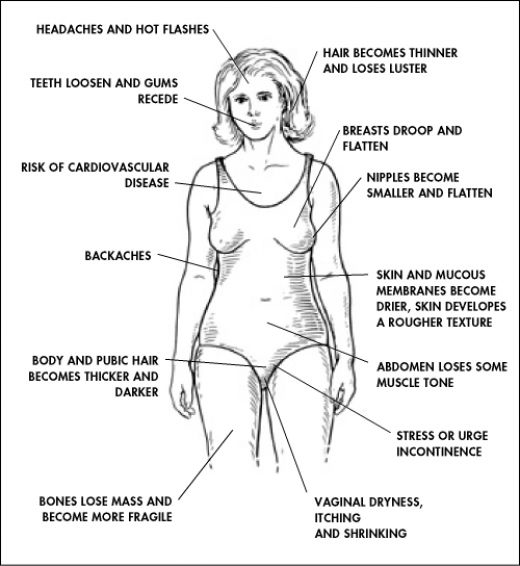
What are the possible symptoms and problems of the menopause?
The menopause is a natural event. You may have no problems. However, it is common to develop one or more symptoms which are due to the low levels of oestrogen.
-
VASOMOTOR SYMPTOMS
-
Hot flushes occur in about 3 in 4 women. Hot flushes may occur at any time of day or night and can be precipitated by a variety of common situations such as sleeping, working, recreation, housework or stress. Flushes usually begin in the face, neck, head or chest. Hot flushes may be associated with episodes of sweating, elevation of skin temperature, irritability, lethargy, insomnia and chronic tiredness. Successful treatment of hot flushes will usually relieve associated symptoms of exhaustion and depression. The number of hot flushes can vary from the occasional flush, to fifteen or more times a day. They may be more abrupt and more severe in women whose menopause is induced suddenly, by surgery or radiotherapy. Hot flushes tend to start 3 to 4 years before the menopause, and typically persist for 2-3 years after menopause.
Potential hot flush triggersAlchohol Hot drinks Spicy foods Hot environment Stress Caffeine
Overweight(BMI>30) Excessive, strenuous activity -
Sweats (hot flushes that occur at night) commonly occur when you are in bed at night. In some cases they are so severe that sleep is disturbed and you need to change bedding and night clothes
-
-
VAGINAL AND URINARY TRACT CHANGES
Estrogen deficiency as a result of menopause leads to atrophic changes and reduced blood flow in the genital tract and urethra. Vaginal tissues become thinner and drier with menopause and therefore become more susceptible to irritation and infections The consequences of these changes are increasing dyspareunia(painful intercourse) and, genital tract trauma, loss of libido, vaginitis and vaginal infections, voiding difficulties, painful urination, increased urinary frequency, urgency and incontinence, recurrent urinary tract infections.
Estrogen treatment (through Hormone Replacement Therapy) could also reverse vaginal atrophy.
-
PSYCHOLOGICAL CHANGES AND MOOD DISTURBANCES.
 Menopause causes many psychological changes in women. Anxiety, irritability
and depression are some of the common psychological changes occurring in
women, in menopause. Other causes of depression may also occur at the time of
menopause. These include loss of reproductive potential, a perceived loss of
femininity, marital disenchantment, the 'empty nest' syndrome and career
disappointments.
Menopause causes many psychological changes in women. Anxiety, irritability
and depression are some of the common psychological changes occurring in
women, in menopause. Other causes of depression may also occur at the time of
menopause. These include loss of reproductive potential, a perceived loss of
femininity, marital disenchantment, the 'empty nest' syndrome and career
disappointments.
-
SLEEP DISTURBANCES
 Sleep problems include waking up more often than normal,increased night
awakenings, tossing and turning all night, just a general inability to get to
sleep. The time it takes to fall asleep is longer than when the woman was
younger. Total length of time asleep is shorter. Typically, the occurrence of
insomnia doubles during menopause than experienced normally before menopause.
Sleep problems include waking up more often than normal,increased night
awakenings, tossing and turning all night, just a general inability to get to
sleep. The time it takes to fall asleep is longer than when the woman was
younger. Total length of time asleep is shorter. Typically, the occurrence of
insomnia doubles during menopause than experienced normally before menopause.
The sleep disturbances experienced by women around menopause are multifactorial in origin. The sleep disturbances coupled with the psychological changes and depression can cause very severe problems for women like difficulty concentrating at work, memory problems, anxiety, and overall poor quality of life. There are important implications for mood, behavior, and cognitive performance.
-
Weight Gain
Many women experience weight gain as they reach their 40s and 50s. However, this may be due to the natural process of aging - and not solely from menopause. With age, it's harder to maintain muscle mass. Lower muscle mass slows down your metabolism, so it's easier to gain weight.
Weight gain - particularly around the abdomen - is common in women around the years of menopause. The increase in abdominal fat is particularly dangerous, as it ups the risk for heart disease. That's why cutting down on calories, eating a nutritious diet, and taking the time for exercise is so important.
WHAT ARE THE LONG TERM HEALTH PROBLEMS AFTER MENOPAUSE?
-
HEART DISEASE:
Prior to menopause, women have a decreased risk of heart disease and stroke when compared with men. Around the time of menopause, however, a women's risk of cardiovascular disease increases, due to loss of beneficial effects of estrogens
Many women think that heart disease is a man's disease. It isn't. Heart disease is the number 1 killer of women. In fact, after age 50, nearly half of all deaths in women are due to some form of cardiovascular disease. That's more than deaths from all cancers combined.
Estrogen helps protect women against CVD during the childbearing years. Estrogens reduce LDL cholesterol (bad cholesterol), increase HDL cholesterol (good cholesterol), and have various direct and indirect benefits on the heart and blood vessels. Once a woman reaches the age of 50, about the age of natural menopause, her risk for heart disease increases, as the beneficial effects of estrogens are lost. In young women who have undergone early or surgical menopause, who do not take estrogen, their risk for heart disease is also higher. Women who have gone through menopause and also have other heart disease risk factors, such as the following, are at even greater risk. Other heart disease risk factors include:-
Diabetes
-
Smoking
-
High blood pressure
-
High LDL (low density lipoproteins) or "bad" cholesterol
-
Low HDL (high density lipoproteins) or "good" cholesterol
-
Obesity
-
Inactive lifestyle
-
Family history of heart disease
-
-
OSTEOPOROSIS:( BRITTLE BONE DISEASE)
Ostoeporosis is a systemic skeletal disease characterized by low bone mass and microarchitectural deterioration with a consequent increase in bone fragility with susceptibility to fracture' i.e. bone with lower density and higher fragility with higher fracture risk.
Estrogens increase bone mineral density in several ways.-
Estrogens increase calcium absorption from the intestines
-
Estrogens increase calcium deposition into the bones by activating osteoblasts.
-
Estrogens reduce calcium resorption from bones by inhibiting osteoclasts.
Lack of estrogens after menopause results in increased bone resorption and loss of bone mineral density.
Peak bone mass in a woman is achieved at 30-35 years old. After 35 years, bone loss occurs at a rate of 0.5-1% per year. With acute estrogen deficiency after menopause, there is accelerated bone Loss which is about 1.5-2% Loss Of Total Bone Mass/Year. For the first 20 years after cessation of menses, menopause related bone loss results in 50% Reduction In trabecular bone and 30 % reduction in cortical bone, thus making the bones very fragile.(men loose only 25% bone by 85 to 90 years)
-
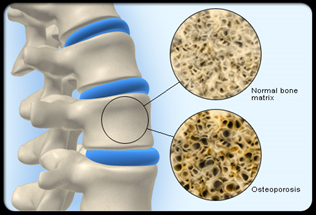
What are the complications of osteoporosis?
The greatest complication associated with osteoporosis is
fractures, which occur most often in the hip, wrist, and spine.
Osteoporosis is associated with fragility fractures that occur in the vertebral
column, rib, hip and wrist. The increased risk of falling associated with aging
leads to fractures of the wrist, spine, and hip. The symptoms of a vertebral
collapse ("compression fracture") are sudden back pain, often with
radiculopathic pain (shooting pain due to nerve root compression) and rarely
with spinal cord compression or cauda equina syndrome. Multiple vertebral
fractures lead to a stooped posture, loss of height, and chronic pain with
resultant reduction in mobility. Fractures of the long bones acutely impair
mobility and may require surgery. Hip fracture, in particular, usually requires
prompt surgery, as there are serious risks associated with a hip fracture, such
as deep vein thrombosis and a pulmonary embolism, and increased mortality.
What are the risk factors for Osteoporosis?
-
Non modifiable: advanced age, family history of fracture or osteoporosis , estrogen deficiency following menopause or oophorectomy.
-
Modifiable : Excess alcohol, tobacco smoking, low dietary calcium and/or phosphorus, vitamin D insufficiency, Obesity, Excessive caffeine intake(more than 3 cups coffee/day), Sedentary lifestyle (lack of physical activity)
-
Diseases and medications: Chronic steroidal intake, Heparin treatment, Hypogonadal states.
Skin Changes
Estrogen loss can contribute to slackness and dryness in the skin and wrinkles.
Cognitive Function
Estrogen, the primary female hormone, appears to have properties that protect
against the memory loss associated with normal aging. Many women who are either
perimenopausal or menopausal complain of mild forgetfulness, but estrogen
replacement therapy does not preserve mental function.
MANAGING MENOPAUSE AND AGING GRACEFULLY
The short-term goals of treatment are different from the long-term goals. Short-term therapy is designed to relieve symptoms like hot flushes, vaginitis, psychological changes; long-term therapy helps to prevent bone loss and osteoporosis.
Lifestyle modification--- A must for healthy menopause and graceful aging.
Maintaining a healthy diet and healthy body weight, doing regular physical
activity, limiting alcohol
consumption and not smoking are all lifestyle factors that may help relieve mild
menopause symptoms.
Get regular exercise. Regular physical exercise can keep bones and muscles strong, and improve balance, flexibility and agility. Exercise also helps the heart, slows bone loss, enhances self-esteem, reduces stress and plays an important role in maintaining a healthy weight. An optimal activity plan will combine weight-bearing and aerobic activities, with strength or resistance training, and stretching or yoga for flexibility. Aerobic exercises will improve your cardiovascular health, lower your blood pressure and reduce your risk of suffering from coronary heart disease; whereas resistance training will improve the tone and strength of your muscles and also increase your bone mass, which is important for reducing your risk of developing osteoporosis. You will experience the full range of benefits if you perform regular aerobic and resistance exercise.
Aerobic exercises Aerobic exercises to choose from include brisk walking,
bicycling, dancing, lap swimming, water aerobics or jogging. Select a few
activities you enjoy and alternate them throughout the week. Postmenopausal
women need to complete at least 30 minutes of moderately intense aerobic
activity at a minimum of five days a week. If you're just beginning an exercise
program, start with a goal of 10 minutes of activity and work your way up to 30
minutes. If weight loss is your goal, increase that activity to 60 minutes a day
until you reach your optimal weight.
Aerobic exercises will improve your cardiovascular health, lower your blood
pressure and reduce your risk of suffering from coronary heart disease;




Dancing is a great low-impact exercise that can burn calories and help reduce
your muffin top. Walking at a brisk pace is a great calorie burner and may also
help with mood swings. Swimming is another great aerobic exercise for older
women who aren't used to physical activity. Swimming is especially beneficial to
people suffering from joint or arthritic pain. It works almost all parts of your
body, such as the shoulders, back, abdomen, legs, hips and buttocks, without
placing stress on joints or fragile bones.
Strength-Training Exercises Regular strength training exercises will help to
boost your metabolism to burn more calories and help your bones keep the
minerals they need to stay strong. Reducing bone loss is critical in preventing
osteoporosis and bone fractures, especially during menopause when bone loss
increases. Strength training exercises involve exercises in which your muscles
contract against a force. Common strength training exercises involve machines,
free weights or resistance bands that exercise your arms, shoulders, chest,
back, stomach, hips and legs. When beginning strength-training exercises, start
with a weight that is comfortable for you. Slowly work your way up. Gradually
increase the weight as the exercises become easier.
Yoga. Yoga workout benefits a postmenopausal woman by stretching and
strengthening the muscles to aid in fighting the age-related loss in muscle
mass. Yoga also increases the range of motion in the joints to help keep them
limber and healthy. Other benefits are improved posture, stability and balance,
which may help reduce the risk of falls. Yoga routines focus heavily on working
out your abdominal muscles with a series of twists and crunches that can
effectively trim away the excess belly fat associated with middle age. The slow,
controlled movements of yoga also aids in reducing stress and increasing
relaxation.
There is strong evidence that regular physical activity can also lower your risk of:
- Heart disease
- Stroke
- High blood pressure
- Unhealthy cholesterol levels
- Type 2 diabetes
- Metabolic syndrome
- Colon cancer
- Breast cancer
- Falls
- Depression
Physical activity may also help: - Improve functional health for older adults
- Reduce waistline size
- Lower risk of hip fracture
- Lower risk of lung cancer
- Maintain weight after weight loss
- Increase bone density
- Improve sleep quality
Quit smoking.
If a woman smokes, she should quit. Cigarette smoking also increases the
frequency and severity of hot flashes. Smoking is linked to a decline in
estrogen levels. Women who smoke reach menopause about 2 years earlier than
nonsmokers. Smoking doubles a woman's odds of developing heart disease and is a
major risk factor for osteoporosis.
Dietary Modification:(Basic dietary guidelines for healthy menopause)
Foods to eat
- Drink plenty of water. This will help you stay hydrated. It's impossible to determine how much water we all need, because this depends on many factors such as how much you eat, the climate you live in, and how active you are. As a general rule, drinking eight glasses of water every day fulfills most everyone's daily requirement.
- A diet rich in vegetables and fruits. Vegetables and fruits that are deeply colored (spinach, carrots, peaches, berries) are especially recommended as they have the highest micronutrient content. Fruits and vegetables are excellent sources of fibre, vitamins and minerals, besides being low in fat.
- Choose whole-grain, high-fiber foods. These include fruits, vegetables, and legumes (beans). Good whole grain choices include whole wheat, oats/oatmeal, rye, barley, brown rice, buckwheat, bulgur, millet, and quinoa.
- Eat fish, especially oily fish, at least twice a week (about 8
ounces/week). Oily fish such as salmon, mackerel, and sardines are rich in the
omega-3 fatty acids eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA).
Consumption of these fatty acids is linked to a reduced risk of sudden death
and death from coronary artery disease.
--Calcium and Vitamin . A combination of calcium and vitamin D is important for helping to prevent the bone loss associated with menopause. The standard recommended calcium dose for adults age 50 years and older is at least 1,200 mg per day, depending on risk factors. The recommended daily intake of vitamin D is 600 IU a day after age 50. Drinking milk fortified with vitamin D and sunlight exposure supply most people's need for vitamin D. People with poor dietary calcium and exposure to sunlight need supplementation of calcium and Vit D. Be careful not to get more than 2,000 mg of calcium a day very often. That amount can increase your chance of developing kidney problems. - Include Soy in diet
 Soy contains phytoestrogens, which for some women can improve menopause
symptoms. Beyond these plant estrogens themselves, the isoflavones in soy also
trigger certain women to produce more equol - an estrogen that forms in the
intestine, which can also help naturally treat hot flashes, though some
studies show minimal or no benefit. Hormones aside, soy is a great source of
fiber and some types of tofu also provide calcium. If you substitute soy for
red meat at least twice a week you will tip the balance toward menopause
health.
Soy contains phytoestrogens, which for some women can improve menopause
symptoms. Beyond these plant estrogens themselves, the isoflavones in soy also
trigger certain women to produce more equol - an estrogen that forms in the
intestine, which can also help naturally treat hot flashes, though some
studies show minimal or no benefit. Hormones aside, soy is a great source of
fiber and some types of tofu also provide calcium. If you substitute soy for
red meat at least twice a week you will tip the balance toward menopause
health.





Foods to avoid
- Limit Alchohol. Excess alcohol can trigger hot flushes, Increase risk for heart disease and osteoporosis
- Avoid hot drinks, spicy foods, excess caffeine (> 2 cups coffee) which can trigger hot flushes
- Use little or no salt in your foods. Reducing salt can lower blood pressure and decrease the risk of heart disease and heart failure.
- Cut down on beverages and foods that contain added sugars (corn syrups, sucrose, glucose, fructose, maltrose, dextrose, concentrated fruit juice, honey).
- Reduce foods high in Fats. Limit daily intake of saturated fat (found mostly in animal products) to less than 7% of total calories, trans fat (found in hydrogenated fats, commercially baked products, and many fast foods) to less than 1% of total calories, and cholesterol (found in eggs, dairy products, meat, poultry, fish, shellfish) to less than 300 mg per day. Choose lean meats and vegetable alternatives (such as soy). Select fat-free and low-fat dairy products. Grill, bake, or broil fish, meat, and skinless poultry.




Management of Vasomotor symptoms
Regular aerobic exercise can help decrease hot flashes. However, excessive
exercise may worsen hot flashes. Weight control- normal healthy weight women
have fewer hot flushes compared with overweight women. Avoid certain foods that
may cause sweating (such as spicy foods, alcohol, and excess caffeine). Keep
your bedroom cool and well-ventilated. Women troubled by hot flashes should
dress in layers, so that they can be removed easily. Maintain a regular bedtime
schedule
Estrogen replacement therapy (ERT) and hormone replacement therapy (HRT) have
clearly been
shown to be an effective treatment for hot flashes. Taking ERT/HRT on a
short-term basis (1-5years) may be a good strategy for women whose primary
concern is hot flashes. Always start ERT or HRT only under supervision and
guidance of your gynecologist.
Several clinical trials have demonstrated a mild but significant improvement in
hot flashes with dietary phytoestrogen supplementation (e.g., soy products).
Clonidine, bellergal, and low dose oral contraceptives (20 mcg estrogen) have
been shown to reduce the incidence of hot flashes. Oral contraceptives have the
added benefit of regulating menses and preventing unintended pregnancy in
perimenopausal women.
Management of vaginal and urogenital symptoms
Conjugated estrogen cream for vaginal application, an intravaginal sustained-release estradiol ring, or estradiol vaginal tablets are recommended as effective treatment for vaginal atrophy. Patients with recurrent urinary infections also benefit from vaginal estrogen cream.
Vaginal lubricants may be recommended for subjective symptom improvement of dyspareunia (painful intercourse) and make intercourse more comfortable and regular sex may help the vagina maintain its elasticity.
Strategies for Preventing Diseases of Advancing Age and aging gracefully
Strategies for preventing the diseases associated with advancing age can be multi-faceted, and include dietary, exercise, and possibly lifestyle changes as well as pharmacologic interventions. Counseling should consider the broad range of pharmacologic and non-pharmacologic interventions that can address the health considerations under discussion at the time of menopause. Counseling should also include the strength of the supporting scientific evidence for each of the interventions.
Most pharmacologic approaches to managing menopause carry risks as well as benefits. A clinician must have a thorough understanding of a patient's own and her family's histories of cancers, heart and cardiovascular disease, osteoporosis, and other conditions that may influence her inherent risk of developing disease or the degree to which a pharmacologic intervention might increase (or decrease) her risk.
Coronary Heart Disease
Coronary heart disease (CHD) is the leading cause of death and a significant cause of morbidity in American women. The risk of CHD increases in older women. Although many women fear breast cancer more than heart disease, one in two women will eventually die of heart disease or stroke, while only one in 25 will die from breast cancer. or has other non-cardiac vascular disease
What are the Possible Interventions for Prevention and/or Treatment of CHD?
Women should:
- Incorporate regular physical activity into their daily routines.
- Achieve and maintain desirable weight and body mass index (BMI). (BMI equals weight in Kilograms divided by height in meters, squared. A BMI of 25-29.9 is considered overweight; a BMI of 30 or more is considered obese.)
- Learn stress management techniques.
- Quit smoking
- Eat a healthful diet, i.e., one low in fat, cholesterol, and salt, and high in dietary fiber.(see dietary modifications above)
- Consume adequate amounts of vitamins C and E (antioxidants that may help reduce the deposition of LDL in the arteries).
- Achieve and maintain a blood pressure <140/90 mm Hg (optimal = <120/<80)
-
Normalize lipid levels based on risk factors:
-
total serum cholesterol < 200 mg/dL
-
LDL < 130 mg/dL (or < 160 mg/dL, depending on other risk factors)
-
HDL ( 35 mg/dL
-
Triglycerides < 160 mg/Dl
-
OSTEOPOROSIS
What are the possible Interventions for Prevention and/or Treatment of Osteoporosis?
Women should:
- Be counseled on risk factors for osteoporosis.
- Obtain an adequate intake of dietary calcium (at least 1,200-1,500 mg per day). (Note: TheNational Institutes of Health believe that daily intake approaching or exceeding 2,000 mg is more likely to cause adverse effects than lower intakes.)
- Obtain an adequate intake of vitamin D (400 to 800 IU per day). Most women
will get their recommended daily allowance through diet and exposure to
sunlight; others can use
supplements. - Do regular weight-bearing and muscle-strengthening exercise. These
exercises improve
bone health, strengthen muscles, and improve balance (which will help prevent falls). - Be counseled on fall prevention (e.g., taping down rugs, using night lights, etc.).\
- Stop smoking.
- Keep alcohol intake moderate (i.e., a maximum of one drink per day, which equals 12 oz.beer, 5 oz. wine, or 1.5 oz. liquor.)
- Be evaluated for osteoporosis with bone mineral density (BMD) testing if:
they are postmenopausal and present with fractures.- Consider BMD testing if:
- They are postmenopausal, under 65, and have one or more additional
risk factors for
osteoporosis (besides being Caucasian); - They are 65 or older, regardless of additional risk factors; or
- Their decision to begin taking ERT/HRT or other treatment would be influenced by the BMD result.
- Be considered candidates for osteoporosis treatment if they present with vertebral or hip fractures or their BMD T-scores are below -2 in the absence of risk factors, or below -1.5 if other risk factors are present
Medications for prevention and treatment of osteoporosis
ERT/HRT
ERT/HRT is effective for the prevention and treatment of postmenopausal osteoporosis for the duration during which it is used. It prevents bone loss in women in the early and late postmenopause. Epidemiologic studies of ERT/HRT indicate a 50-80% decrease in vertebral fractures and a 25% decrease in nonvertebral fractures with five years or more of use, and an anticipated 50-75% decrease in all fractures with 10 or more years of use. Based on effectiveness and other potential benefits, it provides the greatest benefit relative to cost (although potential risks and patient preferences must be taken into account).
Alendronate
This bisphosphonate has been approved for prevention and treatment of osteoporosis. It inhibits bone loss in postmenopausal women, and increases BMD and decreases the risk of fracture in patients with osteoporosis. Well-conducted, controlled clinical trials indicate that alendronate reduces the risk of fracture at the spine, hip, and wrist by 50% in patients with osteoporosis.
Raloxifene
Raloxifene, a SERM, has been approved for the prevention and treatment of osteoporosis. It inhibits bone loss, and preliminary data in women with osteoporosis show that it reduces the risk of vertebral fracture by about 40-50%. It is less effective than ERT/HRT, alendronate, or risedronate.
Calcitonin
Salmon calcitonin, a hormone that inhibits bone resorption, is delivered as a single daily intranasal spray. It is recommended for women greater than five years postmenopausal with low bone mass relative to healthy premenopausal women. Efficacy data for calcitonin are currently weaker than for ERT/HRT, alendronate, or risedronate. (Results from a single controlled clinical trial indicated that it may decrease vertebral fractures by about 40%.)
Risedronate
This bisphosphonate is reported to be as effective as alendronate and did not cause more esophageal irritation than placebo in a randomized clinical trial. (FDA approval is anticipated in 2000.)
Nonprescription
Soy/Phytoestrogens
Randomized clinical trials using a potent synthetic phytoestrogen derivative (ipriflavone) demonstrated a positive effect on bone density, although doses were much higher than achievable through dietary phytoestrogen intake (ipriflavone is not available in the U.S.). There is no data on fracture reduction. More research is needed.24
Stroke
Following the guidelines above for prevention of CHD will also decrease a woman's risk of stroke. Evidence is inconsistent on the preventive effect of ERT/HRT on stroke.
Alzheimer's Disease
There is some evidence that ERT/HRT may be protective against cognitive decline and the incidence of Alzheimer's disease, but further study is required. It does not seem appropriate at this time to use ERT/HRT solely for the prevention or treatment of dementia and cognitive decline.
- They are postmenopausal, under 65, and have one or more additional
risk factors for
- Consider BMD testing if: