ECTOPIC PREGNANCY
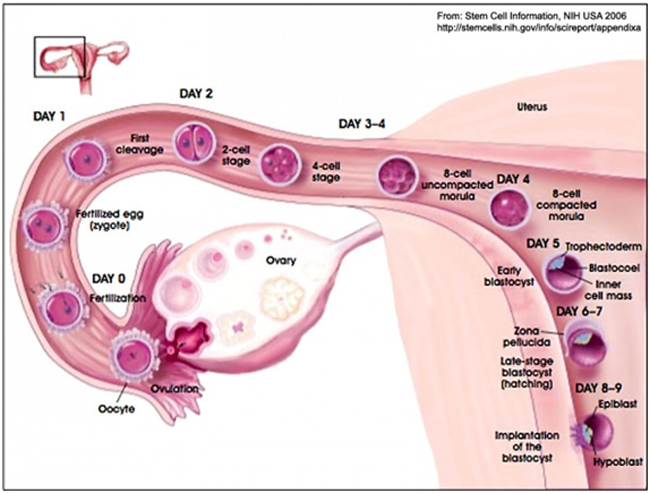
An ectopic pregnancy, is a complication of pregnancy in which the embryo implants outside the uterine cavity. In a normal pregnancy, the fertilized egg enters the uterus and settles into the uterine lining where it has plenty of room to divide and grow.
Ectopic pregnancies are not viable. They are dangerous for the mother, since internal haemorrhage is a life-threatening complication. An ectopic pregnancy is a potential medical emergency, and, if not treated properly, can lead to death. Ectopic pregnancy is a major cause of pregnancy related deaths in the first trimester.
Fig: Normal fertilization, transport of fertilized egg through tube, and implamtation in uterus
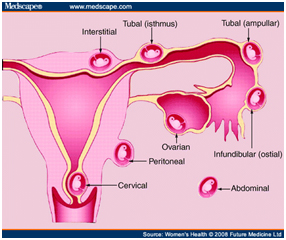
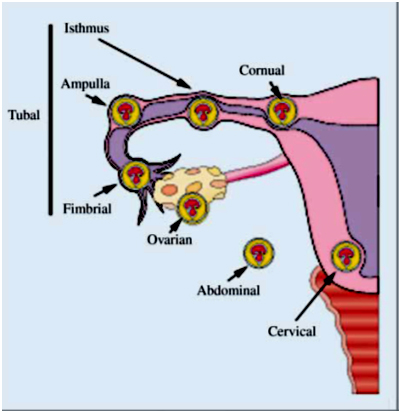
Sites of Ectopic Pregnancy:
Most ectopic pregnancies occur in the Fallopian tube (so-called tubal pregnancies), but implantation can also occur in the cervix, ovaries, and abdomen.
Causes of Ectopic Pregnancy:
Ectopic pregnancy may occur without any cause or risk factor
An ectopic pregnancy is often caused by a condition that blocks or slows the movement of a fertilized egg through the fallopian tube to the uterus. Any disruption of the normal architecture of the Fallopian tubes can be a risk factor for a tubal pregnancy Such causes include:
A) Congenital( birth defects of the fallopian tube)
B) Acquired:
- 1) Pelvic inflammatory disease, -Caused either by sexually transmitted disease or infections from the surrounding organs like appendicitis. Infection causes an ectopic pregnancy by damaging or obstructing the Fallopian tubes. Sexually transmitted infections , especially those caused by gonococci and Chlamydia are notorious in causing tubal damage. They damage the normal lining of the tube, cause intratubal adhesions(blockage within the tube), scarring and narrowing of the tube. Normally, the inner lining of the Fallopian tubes is coated with small hair-like projections called cilia. These cilia are important to transport the egg smoothly from the ovary through the Fallopian tube and into the uterus. If these cilia are damaged by infection, egg transport becomes disrupted. The fertilized egg can settle in the Fallopian tube without reaching the uterus, thus becoming an ectopic pregnancy. Because having multiple sexual partners increases a woman's risk of pelvic infections, multiple sexual partners also are associated with an increased risk of ectopic pregnancy
- 2) Previous surgery on the Fallopian tubes: a) Recanalisation (reunion of fallopian tubes after ligation) increases the risk of fallopian tubes.
- 3) Prior history of an ectopic pregnancy. The recurrence rate is 15% after the first ectopic pregnancy, and 25 % after the second.
- 4) Intra -Uterine device(IUD): The number of women becoming pregnant with IUD in situ are very less, hence the overall ectopic pregnancy rate with IUD usage is very low.But if there is a pregnancy with IUD in situ, The chance of ectopic pregnancy are very high(33%, 1 in 3 women)
- 5) Endometriosis: The adhesions seen in endometriosis can narrow the Fallopian tubes and disrupt egg transportation, thereby increasing the chances of an ectopic pregnancy.
- 6) Assisted reproductive techniques have also been suggested to have increased the incidence of ectopic pregnancy
- 7) Cigarette smoking: The risk associated with smoking increased in a dose-dependent manner. This is probably a causal relation , and tobacco use may play a role at various stages in reproduction: ovulation, fertilization, viability, and implantation. Smoking cessation reduces the risk of ectopic pregnancy to a level intermediate between that of current smokers and that of women who have never smoked.
- 8) Prior Spontaneous Abortions: The risk of ectopic pregnancy high in women with three or more previous spontaneous abortions. Spontaneous abortions may have a causal effect, possibly mediated by infection.
b) Tubal sterilization. Tubal sterilization actually reduces the chances of pregnancy. If pregnancy occurs despite sterilization (occurs in only 0.1% of cases), the chances of ectopic pregnancy is higher.
Differential Diagnosis of Ectopic Pregnancy
| Conditions related to pregnancy. | Conditions not related to pregnancy |
|---|---|
| 1) Threatened abortion | 1) Appendicitis |
| 2) Incomplete abortion | 2) Pelvic inflammatory disease |
| 3) Complete Abortion | 3) Renal calculus |
| 4) Molar pregnancy | 4) Twisted ovarian cyst/ pedunculated fibroid |
| 5) Ruptured ovarian cyst |
MANAGEMENT OF ECTOPIC PREGNANCY:
Management of unruptured ectopic pregnancy: Once ectopic pregnancy is diagnosed, it has to be treated with utmost urgency, as any delay in treatment may result in rupture and may prove to be fatal. Unruptured tubal ectopic pregnancy can be managed either with medical management of Surgery
Medical management of unruptured ectopic pregnancy: Methotrexate injection is used in the medical management of unruptured ectopic pregnancy. Methotrexate is a drug that was initially used to treat unique cancers, some of which were derived from placental tissue.It is a Folic Acid antagonist, and very toxic to rapidly dividing cells like placental tissue. It is very effective in destroying ectopic pregnancy tissue and allowing it to be re-absorbed by the body.
Medical management of ectopic pregnancy cannot be offered to all the patients. Medical therapy should be offered to suitable women, and units should have treatment and follow-up protocols for the use of methotrexate in the treatment of ectopic pregnancy.
The patients to be selected for medical management with methotrexate should meet the following criteria
- 1) Unruptured tubal ectopic with a hemodynamically stable patient, with no signs of rupture(no evidence of internal bleeding and severe pain)
- 2) Normal baseline liver and renal function tests
- 3) Ectopic mass less than 4 cms on transvaginal ultrasonography
- 4) Cardiac activity(heart beats) should be preferably absent
- 5) Serum bHCG should be preferably <5000mIU/ml
When the above criteria are met, the success rates in the treatment of unruptured ectopic is similar to the success rates achieved with conservative surgery.
Patients selected for medical management should have commitment for complete follow up until the ectopic is fully resolved. Patients should also be explained that a surgical treatment may be required if the ectopic pregnancy ruptures during the course of medical treatment or if the ectopic pregnancy fails to resolve (as indicated by blood tests)
The patient also needs to maintain communication with her physician during the treatment protocol and return for follow-up blood tests after treatment.
Absolute contraindications of medical management with methotrexate:(never to be used)
- 1) Evidence of ruptured ectopic(ultrasonography showing internal bleeding or severe abdominal pain)
- 2) Renal or hepatic dysfunction
- 3) Blood dyscrasias
- 4) Active pulmonary disease
Relative contraindications : ( to be used with caution)
- 1) Ectopic mass > 4cms on ultrasonography
- 2) Serum bHCG > 5000mIU/ml
- 3) Presence of fetal cardiac activity
In the above cases of relative contraindications, Methotrexate may be given with extreme supervision, as the chances of failure are much higher in these patients.
Treatment Protocol and Dosage of Methotrexate
Usually a single dose protocol of methotrexate is used. Multiple dose protocols are also used by some.
Single dose protocol: Day 0-Blood tests done(Renal function tests, Liver fuction tests, bllod counts, bHCG.
- Day 1--- INJ METHOTREXATE 50 mg/m2 body surface area intramuscularly
- Day 4 and Day 7--- Repeat bHCG levels in blood
If Difference in bHCG level on day 4 and day 7 > 15%-- Repeat bHCG weekly till they come to normal( < 15mIU/ML)--- May take upto 6-8 weeks
If difference in bHCG level on day 4 and day 7 < 15%-- Repeat Inj Methotrexate 50 mg/m2 body surface area and begin new day 1 and do same follow up on day 4 and day 7.
If the patients blood group is Rh negative, than 50 micrograms of inj. Anti-D are give to prevent the risks of isoimmunisation.
Maximum 3 doses of methotrexate may be repeated. If there is no significant fall in bHCG despite 3 doses, or if there is evidence of rupture (internal bleeding) during the course of treatment------- Surgical treatment is required
The patient should be extremely compliant and should be available for follow up for the entire course of treatment till the bHCG levels come back to normal. The patient should also be advised to follow up immediately if she has severe abdominal pain, giddiness or fainting episodes, as this may signify rupture of ectopic pregnancy.
Precautions during methotrexate treatment:
- 1) Avoid intercourse till bHCG level comes back to normal
- 2) Avoid fresh pregnancy till bHCG comes back to normal and for 3 months after that due to the potential teratogenic effects of methotrexate.
- 3) Patients should have ample fluids during treatment period
- 4) Avoid alchohol during treatment
- 5) Avoid Folic acid during treatment
Treatment effects of methotrexate :
Some patients may experience low pelvic pain and little bleeding per vagina during the after methotrexate injection. The ultrasound may also show a slight increase in the size of the ectopic mass due to separation of the ectopic mass from the tubal lining ad subsequent little bleeding within the tube. This may be misinterpreted as signs of ruptured ectopic. But these, are transient and mild , unlike ruptured ectopic when the patient complains of severe abdominal pain, giddiness and internal bleeding demonstrated by ultrasonography. Sometimes, patients may require admission for observation and subsequent trasvaginal ultrasound to differentiate between ruptured ectopic and the separation pain after methotrexate.
Predictors of methotrexate failure:
- 1) Size of gestational ectopic mass> 4 cms on TVS
- 2) Presence of cardiac activity
- 3) Initial bHCG > 5000mIU/ml
- 4) Continuous rapid rise in bHCG during methotrexate treatment.
- Resolution of the ectopic has been reported in about 70-95% of cases treated. This depends somewhat on selection criteria for the study.
- Tubes are later found to be open on the same side as the ectopic by a "dye test" or hysterosalpingogram in 70-85% of cases
- Pregnancy rates and repeat ectopics are comparable to those after conservative surgery
Side effects of methotrexate:
Nausea, vomiting, gastritis, stomatitis, dizziness. Serious complications like neutropenia, bone marrow depression are very rare with single dose therapy.
Surgical treatment of unruptured ectopic
Indications for surgical treatment :
- Impending rupture of ectopic pregnancy
- Contraindications to methotrexate
- Coexisting intrauterine pregnancy
- Not able or willing to comply with medical therapy post-treatment follow-up
- Lack of timely access to a medical institution for management of tubal rupture
- Desire for permanent contraception
- Known tubal disease with planned in vitro fertilization for future pregnancy (only in patients who are otherwise good candidates for surgical therapy)
- Failed medical therapy
Advantages of laparoscopic surgery V/S Open surgery:
- 1) Shorter operating time
- 2) Less intraoperative blood loss(ie : blood loss during surgery)
- 3) Shorter duration of hospital stay.
- 4) Less analgesic requirement.
- 5) Lower chances of repeat ectopic pregnancy.
- 6) Fewer postoperative adhesions.
Operative Procedures in unruptured ectopic pregnancy:
- 1) Salphingostomy ( Tube is cut open over ectopic, ectopic is removed, and cut is left open to heal )--- Tube is preserved
- 2) Salphingotomy(Tube is cut open over ectopic, ectopic is removed, and cut is sutured)-Tube is preserved
- 3) Salphingectomy (Removal of the tube)
If fertility is desired, then linear salphingostomy is the procedure of choice, specially if the other tube is also damaged. In this procedure, the linear incision is given on the antimesenteric border of the tube over the ectopic, the ectopic pregnancy is removed, tube flushed, and the incision is left open to heal by secondary incision. Salphingotomy is also the same procedure, the only difference is that the incision on the tube is sutured.
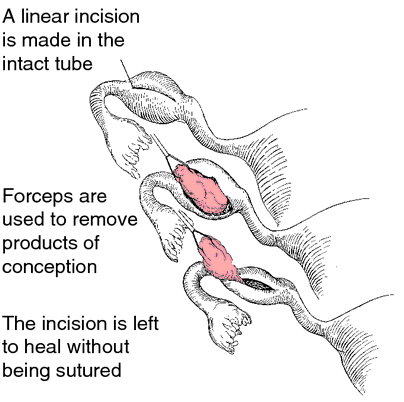
Salphingostomy-Technique
Salphingectomy:(Removal of the tube)
Salphingectomy is often performed, particularly if:
- 1 ) The tube is severely damaged
- 2) There is uncontrolled bleeding
- 3) There is a recurrent ectopic pregnancy in the same tube
- 4) There is a large tubal pregnancy of >5cm
- 5) The woman has completed her family and no longer desires fertility.
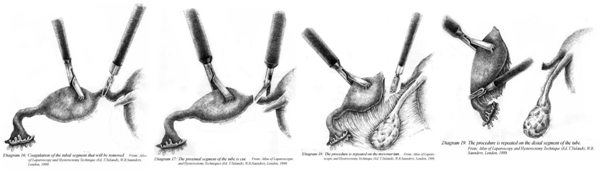
Salphingectomy Technique
In patients with a healthy contralateral tube, whether to do a salphingostomy and preserve the tube, or to do a salphingectomy (removal of tube) is a matter of debate. Salpingostomy preserves the tube, but bears the risks of both persistent trophoblast and repeat ipsilateral tubal EP (repeat ectopic pregnancy in the same tube). Salpingectomy, avoids these risks, but leaves only one tube for reproductive capacity. Some studies have shown that the subsequent intrauterine pregnancy rates after saphingostomy and salphingectomy are similar, but the was a higher recurrent ectopic pregnancy rate on the same side after salphingostomy. Hence, it may not be wrong to perform a salphingectomy (removal of the tube) for unruptured tubal ectopic if the other side tube appears healthy, specially if the patient does not have history of infertility.
In patients with an unhealthy contralateral tube, Salphingostomy(preservation of the tube) is the procedure of choice.
II) Management of Ruptured ectopic pregnancy
Ruptured ectopic pregnancy is a medical emergency, which if not treated in time will result in death of the patient due to internal bleeding. The treatment of ruptured ectopic pregnancy is stabilization of the patient and surgery. Salphingectomy (removal of the tube) is always performed as the ruptured tube cannot be repaired and preserved. There is no role for medical treatment in ruptured ectopic pregnancy.
A) In a Hemodynamically stable patient
If the patient is hemodynamically stable and not in shock, Laparoscopic surgery is preferred. Laparoscopic salphingectomy is performed . Depending on the amount of intraperitoneal hemorrhage, blood transfusion may be required.
B) In Hemodynamically unstable patient(patients in shock)
The patients are to be attended with utmost urgency as there is very little time available for their management. Any delay in the management can result in death of these patients. Their management includes
1) Immediate resuscitation:
- -2 IV lines with 18 g Jelco to be secured
- -Blood transfusion as soon as possible, to replace the blood lost as a result of internal hemorrhage. The number of units of blood required depends upon the degree of internal hemorrhage and the vitals(pulse, blood pressure and circulation) of the patient
- -Till blood is made available, the circulation and blood pressure has to be maintained by intravenous fluids.
2) Emergency surgery:
- -Open surgery is prefered in these patients with shock, as the principle in these patients is "Quick in and quick out".
- -Sometimes, blood availability take time, or blood may not be available. Surgery should not be delayed in these patients, as these patients continue to loose blood due to ruptured ectopic. Hence the only way to save these patients is by emergency surgery (salphingectomy), which stops the internal hemorrhage.